About a month ago, health officials announced the discovery of an Indian “superbug,” otherwise-common bacteria carrying profound resistance to nearly every antibiotic available. This “superbug” isn’t a single particular type of bacterium; rather, it’s a host of different bacteria that all possess a specific gene, called NDM-1 (short for New Delhi metallo-beta-lactamase), that confers “dire” resistance factors on whatever bacteria happen to possess it. A recap from Wired Science:
NDM-1 was first spotted in 2008,
in a 59-year-old man of South Asian origin who lived in
Sweden. He was
hospitalized on a visit home to New Delhi, had surgery, recovered, went
back to Sweden and was hospitalized there again. At that point,
physicians recognized that he had a urinary tract infection that was
unusually drug-resistant. The infection was caused by a common
bacterium, Klebsiella pneumoniae, but the Klebsiella
possessed an unusual and worrisome ability to disable carbapenems, a
class of drugs given for very resistant infections. They named the
enzyme and the gene directing its production for the place where the man
had apparently acquired it: New Delhi metallo-beta-lactamase, and blaNDM.
In 2009, the United Kingdom’s public-health agency sent out an alert
saying the same resistance mechanism was appearing there and increasing
rapidly, going from unknown in 2007 to 18 instances in the first half
of 2009, most of them in people who had gone to India for medical care
or had frequent family travel back and forth. In June this year, the US
Centers for Disease Control and Prevention put out a bulletin about
NDM-1’s first US appearance,
in three patients in three different states (California, Massachusetts
and Illinois), again with ties to South Asian medical care.
It turns out that bacteria carrying the NDM-1 gene have spread around the world. Meanwhile, home-grown superbugs with resistances of their own have been found in 35 different states. Even more troubling: they render ineffective even our “last ditch” treatments for other infections that won’t respond to standard antibiotics. From USA Today:
“We’ve lost our drug of last resort,” Fishman [director of infection control and epidemiology at the University of
Pennsylvania and president of the Society of Healthcare Epidemiologists] says.
Doctors say the bacteria are more worrisome than another well-known
superbug, methicillin-resistant Staphylococcus aureus (MRSA), because
more drugs are available to treat MRSA, Fishman says. “When MRSA started
to develop 15 years ago, the industry started producing antibiotics now
coming onto the market,” he says. “We’re in the same position with KPCs
as we were with staph aureus 15 years ago, except that the
pharmaceutical industry isn’t rushing to produce new drugs.”
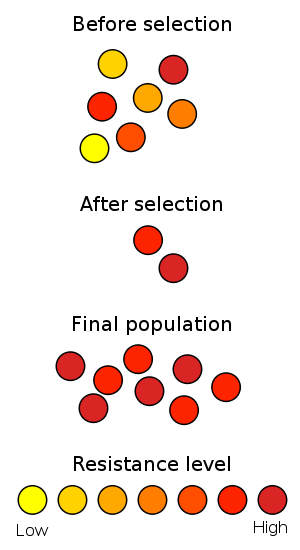
Perhaps we shouldn’t be surprised. Scientists, scholars, and other whistle-blowers have been warning us for some time that our overuse of antibiotics – particularly on factory farms, where drugs are dispensed en masse to healthy animals to prevent infections in unsanitary conditions – could give rise to something particularly nasty. Really, you could call this a classic tale of scientific overreaching – like Frankenstein’s monster, our hubris is coming back to haunt us.
It turns out this is exactly what is happening: Minnesota, one state that is currently beset by its own set of drug-resistant superbugs, tracked their origin to livestock production facilities.
Now, it’s easy to dismiss all of this with a wave of the hand. “So we’ve got these so-called superbugs – big deal, it’s just the new H1N1, which was the new SARS, which was the new…” ad infinitum. Maybe, but maybe not – things get unsettling when we venture into the realm of drug resistance. And you can’t be too careful – it’s better to avoid a devastating global pandemic, as I always say.